马上注册,结交更多好友,享用更多功能,让你轻松玩转社区。
您需要 登录 才可以下载或查看,没有账号?注册
×
A 44-year-old gentleman with no significant medical or surgical history presented to the emergency department with a three-day history of abdominal pain starting at the epigastric and periumbilical areas, which then started to be localized to the right iliac fossa. The pain was dull, aching, progressive in intensity, and associated with nausea and anorexia. However, there was no associated alteration in bowel habits and no history of vomiting or fever.
On physical examination, he was afebrile, and his BMI was 46 kg/m2. The abdomen was soft and lax, with tenderness and rebound tenderness on the right iliac fossa, which raised the suspicion of acute appendicitis given his clinical presentation. On investigation, the complete blood count was unremarkable. A CT scan of the abdomen performed with intravenous, oral, and rectal contrast showed a right lower abdominal wall hernia sized 11.8 x 7.3 x 14.9 cm, seen lateral to the right rectus muscle. Inferiorly, it was close to the inguinal canal with superior extension at the level of the iliac crest, containing parts of the terminal ileum, the ileocecal valve, and the base of the cecum (Figure 1).
Figure 1. CT of the abdomen.
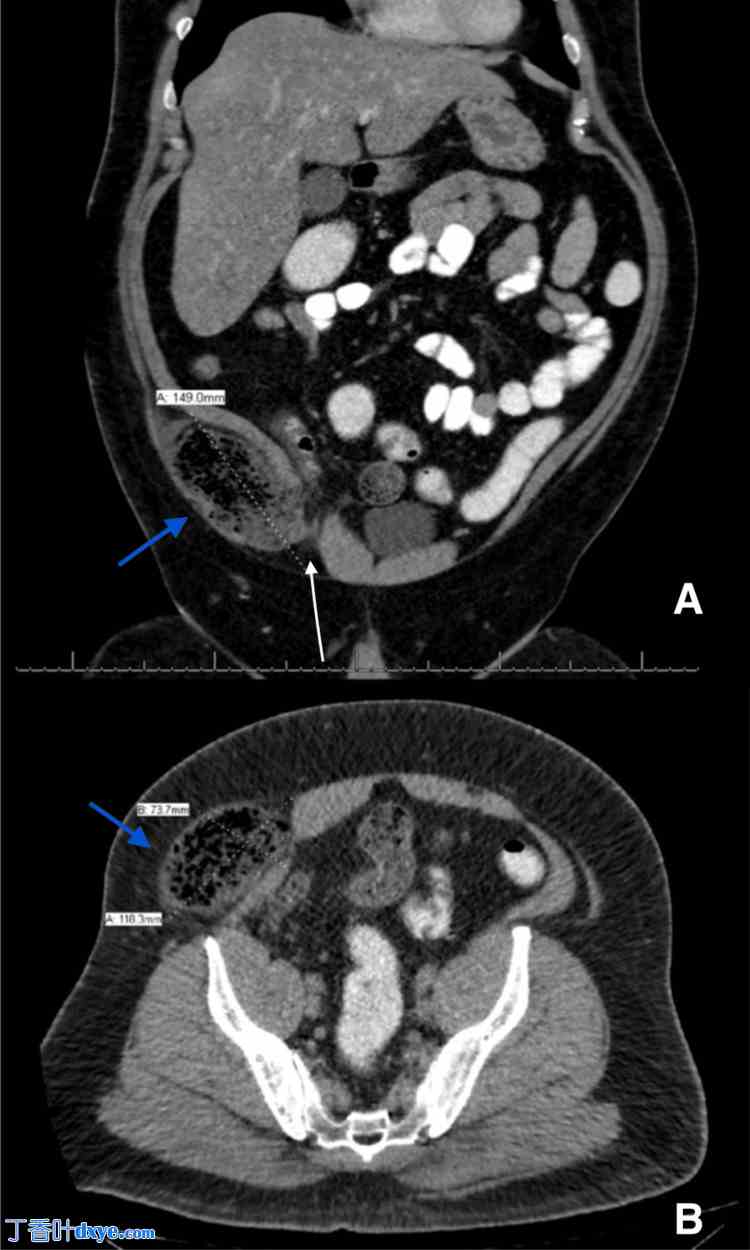
A: Coronal cut of the abdominal CT scan showing the incarcerated wall of the cecum, ileum, and appendix (blue arrow points to the herniated bowel) in relation to the inguinal region(white arrow points to the abdominal wall defect); B: Axial cut with similar findings
Herniated bowels were distended and loaded with fecal matter, with no passage of the oral contrast and a collapsed distal colon. The appendix was hardly seen without obvious signs of appendicitis. Due to the CT findings of the incarcerated, potentially strangulated ventral hernia, the patient was taken to the operating room and underwent a diagnostic laparoscopy with hernia repair. During surgery, a large defect was seen through the deep inguinal ring, with a herniated cecum, appendix, ileocecal valve, and terminal ileum (Figure 2).
Figure 2. Intraoperative findings.

A: Herniated cecum, appendix, and terminal ileum (dashed white arrow), large defect identified in the inguinal region (white arrow)
B: The reduction of herniated healthy-looking bowel (dashed white arrow)
C: The hernia sac is seen through the dilated deep inguinal ring (white arrow), lateral to the inferior epigastric vessels, and spermatic cord (dashed black arrow).
The black arrow in A, B, and C points to the medial umbilical fold.
Hernia content was reduced and examined, and due to the healthy, viable bowel, no resection was required. After hernia reduction, the defect was seen lateral to the inferior epigastric vessels, and the spermatic cord was identified on the medial edge of the defect. Transabdominal preperitoneal (TAPP) hernia mesh repair was done with no complications. The patient improved after the surgery and was discharged on the second postoperative day in good condition.
Interparietal hernia is a rare type of hernia, with an incidence of 0.01% to 1.6%, as reported by Lower and Hicken in the largest case series. And it has been classified into three subtypes: superficial, interstitial, and properitoneal (Figure 3) . The interstitial subtype is considered the most frequently encountered of the three subtypes and accounts for 60% of all interparietal hernias . The most common finding of all cases reported previously in patients with no previous abdominal surgeries is the location in the inguinal region. Due to the rarity of the hernia, no clear etiology has been defined in the literature yet .
Figure 3. Types of interparietal inguinal hernias in relation to the abdominal wall structures.
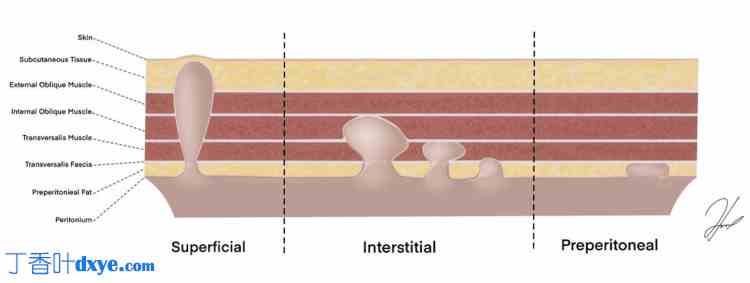
Interparietal hernias classification per Lower and Hicken illustrated by author Alshaaer NEF. |


