马上注册,结交更多好友,享用更多功能,让你轻松玩转社区。
您需要 登录 才可以下载或查看,没有账号?注册
×
概要
背景
肝动脉假性动脉瘤作为腹腔镜胆囊切除术的并发症被认为是一种罕见的,可能危及生命的疾病。
案例介绍
作者报告了在选择性腹腔镜胆囊切除术后复杂胆道和血管损伤后8个月出现迟发性胆道出血的病例。患者通过手术治疗动脉瘤和肝脏吻合术的原发性修复。
结论
当遇到患有大量上消化道出血的患者和之前的肝胆操作或手术病史时,无论术后时间如何,都应该提高怀疑指数。
背景
由于与该病症相关的高发病率和死亡率,血友病和血管损伤是最重要的 - 尽管不一定是腹腔镜胆囊切除术(LC)最常见的并发症[1-3]。胆道出血的症状通常出现在术后早期或最迟4周[3]。除了详细的文献综述外,作者还报告了一例在LC后8个月出现右肝动脉假性动脉瘤并伴有胆总管复杂损伤的病例。据作者所知,文献中有两例类似的病例报告了LC后延迟的肝动脉假性静脉曲张[4,5] [表1]。
表格1
类似病例摘要(腹腔镜胆囊切除术后肝动脉假性动脉瘤)文献报道
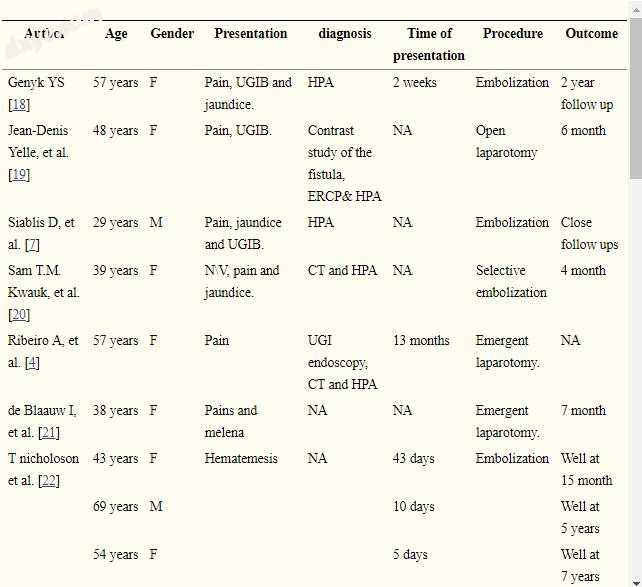
缩写定义:NA不可用,UGIB上消化道出血,HPA肝脏选择性血管造影,ERCP内镜逆行胆管造影,LC腹腔镜胆囊切除术
案例介绍
一名41岁的女性患者出现在作者的急诊室,患有上消化道(UGI)出血史,无痛咖啡磨碎的呕吐物和黑便。除了由于在她出现前8个月在另一个机构中发生急性胆囊炎的远程发作而进行的平稳选择性腹腔镜胆囊切除术之外,患者没有明显的既往病史。在查看患者的图表后,手术顺利,未发生术中并发症,使用单极烧灼能量源,未获得术中胆管造影。
该患者有胆囊切除术后6周出现最小UGI出血的病史,此时上消化道内镜检查和ERCP显示胆道出血,并将支架置于胆总管内。之后,患者症状缓解,CT研究证实存在小的(<0.25 cm)右肝动脉假性动脉瘤。患者可以选择栓塞,但她拒绝接受治疗,并且在当前的介绍中失去了跟进。
在她介绍作者的中心后,患者脸色苍白,心动过速(100-110 bpm)和血压正常。在触诊时注意到腹部柔软且松弛,没有腹膜炎的迹象。
实验室结果
血红蛋白:10.3 g \ L,血细胞比容:33,血小板:44×109 / L.凝血曲线正常,肝功能显示肝酶轻度升高。
患者住院并恢复,之后她准备进行急诊UGI内镜检查,在胃或十二指肠中未发现出血源。然而,注意到血液从主要十二指肠乳头流出,引起怀疑血友病。在ERCP上,旧支架被移位并且在胆总管(CBD)中确定了狭窄,该胆管延伸到肝管但在分叉下方。此外,胆管充满凝块,右肝动脉开始充满对比。将一个塑料支架放在狭窄处(图1)。进行CT腹部血管造影显示右肝动脉的囊状病变提示存在假性动脉瘤(1.5cm)(图2和3).3)。最初在ERCP(支架置入术)后控制出血。不久之后,患者再次恶化,血红蛋白下降至7.7 g \ L,她被转移到重症监护室,用4单位PRBCS和血小板复苏。患者血流动力学稳定并且用于血管造影的血管造影,由于未能插入肝总动脉而未成功。患者继续出现需要进一步输血的胃肠道出血。她被带到手术室进行紧急剖腹探查术。
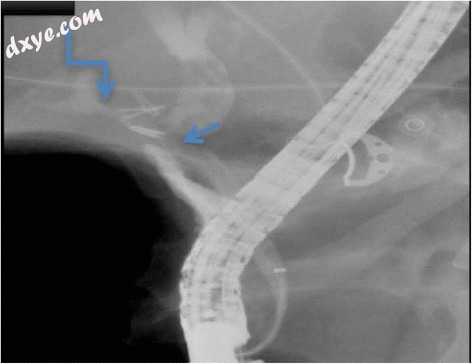
图1
ECRP研究:显示CBD的狭窄(直箭头),冠状动脉充盈缺损和对比填充肝动脉和冠状动脉之间的右肝动脉通路(成角度箭头)
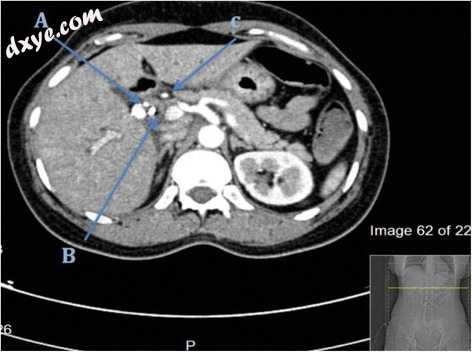
图2
CT研究,轴向切开:箭头指向,A:右肝动脉假性动脉瘤B:支架C:肝总动脉

图3
3D血管造影显示肝动脉动脉瘤(直箭头)
操作说明
通过中线剖腹手术获得腹部探查; 没有腹腔积液的证据。 在获得肝总动脉的近端控制后,难以分离右肝动脉。 肝门区域增厚,水肿可能是由于既往胆管炎和ERCPs所致。 划分CBD以促进右肝动脉的暴露。 然后,将右肝动脉过程分离并控制在假性动脉瘤附近(图4)。 解剖后,动脉瘤意外打开,背部出血最少。 刷新假性动脉瘤壁,并以初级修复方式关闭右肝动脉。
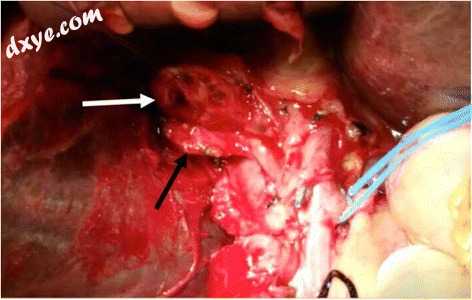
图4
术中:箭头指向,A :(白色)胆总管,B :(黑色)右肝动脉
进行Roux-en-y肝脏 - 颈静脉造口术。支架已经移位并且在横结肠中感觉到,它通过切除术取出。
除伤口感染外,患者恢复良好。她的LFT逐渐恢复到正常水平。出院后患者随访14个月,没有再次出血的证据。
讨论
腹腔镜胆囊切除术(LC)即使在最有经验的外科医生手中也存在胆道和血管医源性损伤的风险。尽管与开放手术相比它具有许多益处,但其使用医源性胆道和血管损伤的风险增加10倍[3]。据报道,腹腔镜胆管系统损伤占0.3-1%,而血管损伤占0.25-0.5%(7-9)。在文献中众所周知,术中出血是LC医源性动脉损伤随后结扎的最常见表现。这里介绍了LC后医源性动脉损伤的不太常见的表现。
所有报告的胆道出血病例中约有10%继发于医源性肝动脉假性动脉瘤(表1)(8)。
上消化道出血是最常见的肝右动脉假性动脉瘤破裂进入胆道。然而,在不到40%的患者中可以看到称为Quinke's triad的胆道出血的典型表现[1,6,7]。
迄今为止,LC后胆道出血的确切病理解释尚不清楚,但建议的机制是机械性,热损伤,特别是腹腔镜手术期间单极凝固和外科夹子侵犯[8-10]。胆汁泄漏和叠加感染是重要的促发因素,据报道,胆汁酸可能导致血管壁损伤,导致血管壁愈合延迟,导致假性动脉瘤的发展[11]。作者认为,由于存在血管和胆道损伤以及她的延迟表现,作者患者的受伤机制是热的。
诊断和控制这种情况有几种选择,上消化道内镜评估是排除UGI出血更常见原因的基础[12]。在目前的文献中,近12%的病例报告通过内镜诊断[13]。
对比增强的腹部计算机断层扫描有助于确定胆道出血的多种病因[14]。诊断胆道出血的困难可能归因于出血通常是间歇性的。
胆道出血的管理是急性紧急情况,因为患者在破裂时可能会放血。治疗目的是阻止出血并重建胆道梗阻[13]。经动脉栓塞(TAE)是所有肝动脉瘤原因的治疗选择,成功率很高,对于选择栓塞试验失败的患者,应进行手术干预(12)。血管造影提供微创手术的优势,它也是这种潜在致命并发症的有效治疗选择[15,16]。
手术范围缩小到需要的条件;胆管修复,肝外病变或胆囊出血,以及TAE失败[15,17]。
在确认胆道出血的诊断和在栓塞缺失或失败的情况下进行外科手术干预的决定之间的时间阶段是至关重要的,并且必须由主治外科医生精心管理。由于这些患者有突然破裂和放血的风险。
结论
所有接受治疗的外科医生都应考虑患有胆道出血病例的患者,当出现上消化道出血并伴有既往胆囊切除术的病史时,无论手术后时期如何。评估肝动脉是所有胆道损伤调查的重要方面。术中预防措施对于预防这些并发症至关重要,例如在LC期间仔细解剖和避免血管 - 胆管结构附近的烧灼使用。
参考:
Delayed hemobilia due to hepatic artery pseudo-aneurysm: a pitfall of laparoscopic cholecystectomy
1. Sandblom P, Saegesser F, Mirkovitch V. Hepatic hemobilia: hemorrhage from the intrahepatic biliary tract, a review. World J Surg. 1984;8(1):41–50. doi: 10.1007/BF01658362. [PubMed] [CrossRef] [Google Scholar]
2. Ross FP. Hemobilia (Biliary Tract Hemorrhage): history, pathology, diagnosis and treatment. Arch Surg. 1973;106(2):245. doi: 10.1001/archsurg.1973.01350140101038. [CrossRef] [Google Scholar]
3. Connor S, Garden OJ. Bile duct injury in the era of laparoscopic cholecystectomy. Br J Surg. 2006;93(2):158–68. doi: 10.1002/bjs.5266. [PubMed] [CrossRef] [Google Scholar]
4. Ribeiro A, et al. Hemobilia due to hepatic artery pseudoaneurysm thirteen months after laparoscopic cholecystectomy. J Clin Gastroenterol. 1998;26(1):50–3. doi: 10.1097/00004836-199801000-00013. [PubMed] [CrossRef] [Google Scholar]
5. Milburn J, et al. Right hepatic artery pseudoaneurysm thirteen months following laparoscopic cholecystectomy. EJVES Extra. 2007;13(1):1–3. doi: 10.1016/j.ejvsextra.2006.09.005. [CrossRef] [Google Scholar]
6. Siablis D, et al. Hemobilia secondary to hepatic artery pseudoaneurysm: an unusual complication of bile leakage in a patient with a history of a resected IIIb Klatskin tumor. World J Gastroenterol. 2005;11(33):5229–31. [PMC free article] [PubMed] [Google Scholar]
7. Siablis D, et al. Hepatic artery pseudoaneurysm following laparoscopic cholecystectomy: transcatheter intraarterial embolization. Hepatogastroenterology. 1996;43(11):1343–6. [PubMed] [Google Scholar]
8. Merrell SW, Schneider PD. Hemobilia--evolution of current diagnosis and treatment. West J Med. 1991;155(6):621–5. [PMC free article] [PubMed] [Google Scholar]
9. Morino M. Randomized clinical trial of ultrasonic versus electrocautery dissection of the gallbladder in laparoscopic cholecystectomy (Br J Surg 2003; 90: 799–803) Br J Surg. 2003;90(10):1306. doi: 10.1002/bjs.4419. [PubMed] [CrossRef] [Google Scholar]
10. Curet P, et al. Hepatic hemobilia of traumatic or iatrogenic origin: recent advances in diagnosis and therapy, review of the literature from 1976 to 1981. World J Surg. 1984;8(1):2–8. doi: 10.1007/BF01658356. [PubMed] [CrossRef] [Google Scholar]
11. Hofmann AF. Bile acids: the good, the bad, and the ugly. News Physiol Sci. 1999;14:24–9. [PubMed] [Google Scholar]
12. Cattan P, et al. Hemobilia caused by a pseudoaneurysm of the hepatic artery diagnosed by EUS. Gastrointest Endosc. 1999;49(2):252–5. doi: 10.1016/S0016-5107(99)70497-9. [PubMed] [CrossRef] [Google Scholar]
13. Napolitano V, et al. A severe case of hemobilia and biliary fistula following an open urgent cholecystectomy. World J Emerg Surg. 2009;4:37. doi: 10.1186/1749-7922-4-37. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
14. Rencuzogullari A, et al. Hemobilia as a result of right hepatic artery pseudoaneurysm rupture: an unusual complication of laparoscopic cholecystectomy. Int J Surg Case Rep. 2014;5(3):142–4. doi: 10.1016/j.ijscr.2014.01.005. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
15. Madanur MA, et al. Pseudoaneurysm following laparoscopic cholecystectomy. Hepatobiliary Pancreat Dis Int. 2007;6(3):294–8. [PubMed] [Google Scholar]
16. Horton KM, Smith C, Fishman EK. MDCT and 3D CT angiography of splanchnic artery aneurysms. AJR Am J Roentgenol. 2007;189(3):641–7. doi: 10.2214/AJR.07.2210. [PubMed] [CrossRef] [Google Scholar]
17. Petrou A, et al. Hemobilia due to cystic artery stump pseudoaneurysm following laparoscopic cholecystectomy: case presentation and literature review. Int Surg. 2012;97(2):140–4. doi: 10.9738/CC52.1. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
18. Genyk YS, Keller FS, Halpern NB. Hepatic artery pseudoaneurysm and hemobilia following laser laparoscopic cholecystectomy. A case report. Surg Endosc. 1994;8(3):201–4. doi: 10.1007/BF00591830. [PubMed] [CrossRef] [Google Scholar]
19. Yelle J-D, et al. Hemobilia complicating elective laparoscopic cholecystectomy: a case report. Can J Surg. 1996;39(3):240–2. [PMC free article] [PubMed] [Google Scholar]
20. Kwauk STM, et al. Traumatic pseudoaneurysm of the hepatic artery after percutaneous liver biopsy and laparoscopic cholecystectomy in a patient with biliary cirrhosis: a case report. Can J Surg. 1998;41(4):316–20. [PMC free article] [PubMed] [Google Scholar]
21. de Blaauw I, van Driel Repelaer OJ. Hemobilia as a complication of laparoscopic cholecystectomy. Ned Tijdschr Geneeskd. 1999;143(47):2380–3. [PubMed] [Google Scholar]
22. Nicholson T, et al. Hepatic artery angiography and embolization for hemobilia following laparoscopic cholecystectomy. Cardiovasc Intervent Radiol. 1999;22(1):20–4. doi: 10.1007/s002709900323. [PubMed] [CrossRef] [Google Scholar]
23. Dogru O, et al. Hemobilia. Surg Endosc. 2003;17(9):1495–6. [PubMed] [Google Scholar]
24. Iannelli A, et al. Hemobilia due to pseudoaneurysm of the right hepatic artery following laparoscopic cholecystectomy. Gastroenterol Clin Biol. 2003;27(3 Pt 1):341–3. [PubMed] [Google Scholar]
25. Roche-Nagle G, Maceneaney, Harte P. Pseudo-aneurysm of the hepatic artery after laparoscopic cholecystectomy: a case report. J Minim Access Surg. 2006;2(2):73–5. doi: 10.4103/0972-9941.26652. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
26. Nakase Y, et al. Hemobilia and cystic artery stump pseudoaneurysm associated with liver abscess after a laparoscopic cholecystectomy: report of a case. Surg Today. 2008;38(6):567–71. doi: 10.1007/s00595-007-3663-9. [PubMed] [CrossRef] [Google Scholar]
27. Masannat YA, et al. A rare complication of a common operation: hepatic artery pseudo aneurysm following cholecystectomy report of a case. Ir J Med Sci. 2008;177(4):397–8. doi: 10.1007/s11845-007-0053-7. [PubMed] [CrossRef] [Google Scholar]
28. Srinivasaiah N, et al. Vascular emergencies in cholelithiasis and cholecystectomy: our experience with two cases and literature review. Hepatobiliary Pancreat Dis Int. 2008;7(2):217–20. [PubMed] [Google Scholar]
29. Yao CA, Arnell TD. Hepatic artery pseudoaneurysm following laparoscopic cholecystectomy. Am J Surg. 2010;199(1):e10–1. doi: 10.1016/j.amjsurg.2009.03.014. [PubMed] [CrossRef] [Google Scholar]
30. Sansonna F, et al. Severe hemobilia from hepatic artery pseudoaneurysm. Case Rep Gastrointest Med. 2011;2011:925142. [PMC free article] [PubMed] [Google Scholar]
31. Liu Z, Yang S, Xi P. An unusual life-threatening hemobilia caused by hepatic pseudoaneurysm following choledochostomy: a case report. Case Rep Clin Med. 2016;5(02):37. doi: 10.4236/crcm.2016.52007. [CrossRef] [Google Scholar]
32. Mate AD, et al. Lower gastrointestinal bleeding due to hepatic artery pseudoaneurysm following laparoscopic cholecystectomy. J Minim Access Surg. 2013;9(1):31. doi: 10.4103/0972-9941.107135. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
33. El Bouhaddouti H, et al. Hemobilia due to an iatrogenic arteriobiliary fistula complicating laparoscopic cholecystectomy: a case report. Open J Gastroenter. 2014;4(06):275. doi: 10.4236/ojgas.2014.46040. [CrossRef] [Google Scholar]
34. Traiki TAB, Madkhali AA, Hassanain MM. Hemobilia post laparoscopic cholecystectomy. J Surg Case Rep. 2015;2015:2. [PMC free article] [PubMed] [Google Scholar]
35. Tun-Abraham M, Martínez-Ordaz J, Romero-Hernandez T. Hepatic artery pseudoaneurysm: report of two cases. Cir Cir. 2013;82(6):674–9. [PubMed] [Google Scholar]
36. Abdalla S, et al. Compressive hematoma Due to pseudoaneurysm of the right hepatic artery: a rare cause of obstructive jaundice after single-port cholecystectomy. Surg Laparosc Endosc Percutan Tech. 2015;25(1):e42–4. doi: 10.1097/SLE.0000000000000024. [PubMed] [CrossRef] [Google Scholar]
37. Hsiao C-Y, et al. Obstructive jaundice as a complication of a right hepatic artery pseudoaneurysm after laparoscopic cholecystectomy. J Minim Access Surg. 2015;11(2):163. doi: 10.4103/0972-9941.144097. [PMC free article] [PubMed] [CrossRef] [Google Scholar] |


